5 Essential Competencies for Practice-Ready Nurses (Plus One That's Surged 165%)

Table of Contents
Name of the heading 1
1- Start your table with the syntax {start-table}
2 - Add an H3 Heading to create a new column (this will be the column title)
3 - List cells as bullet points in a List element
4 - End your table with the syntax {end-table}
Practice readiness is the difference between a new nurse who catches early sepsis and one who doesn't, between a shift that runs smoothly and one where an overwhelmed graduate makes a medication error, and between a nurse who stays at the bedside and one who leaves within a year, crushed by the gap between what they learned and what the job demands.
The cost of that gap compounds fast. Patients face increased safety risks and longer recovery times. Experienced nurses burn out covering for underprepared colleagues. Hospitals pour resources into months-long orientations that still don't bridge the competency divide. And the new graduates themselves—who invested years and often six figures in their education—find themselves drowning in a role they thought they were trained for.
2025 research from UbiSim, which surveyed 390 hospital and health-system hiring leaders across the United States and Canada, puts hard numbers to what frontline staff already know: 65% say it's harder to find practice-ready graduates today than three years ago. The majority agree that new graduates excel at textbook knowledge but struggle when patients don't follow the textbook.
So what exactly separates a day-one ready nurse from one who struggles? The answer comes down to interconnected competencies that have become non-negotiable in healthcare.
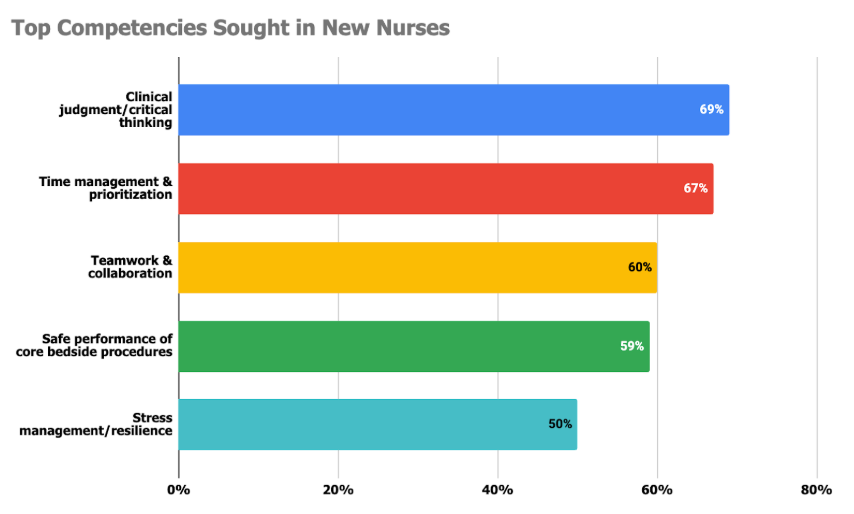
The top 5 competencies hospitals seek:
- Clinical judgment and critical thinking (69%)
- Time management and prioritization (67%)
- Teamwork and collaboration (60%)
- Safe performance of core bedside procedures (59%)
- Stress management and resilience (50%)
#6 Bonus rapid riser: Technology fluency, including AI tools (165% increase in just 3 years)
1. Clinical Judgment and Critical Thinking
When a patient's status starts to shift, there's no time to consult a manual. Clinical judgment—the ability to read between the lines of vital signs, recognize when "stable" is trending toward crisis, and know when to escalate—tops the list at 69%.
Traditional nursing education builds foundational knowledge but falls short on applying it under pressure. It's the difference between knowing textbook sepsis versus noticing a heart rate that's climbed from 88 to 108, flushed skin, and slowed responses at 2 AM in a busy ED.
Sixty-four percent of hiring leaders say new graduates struggle more than experienced RNs to recognize early patient deterioration, the exact skill that prevents a stable patient from becoming a code.
2. Time Management and Prioritization
At 67%, time management is nearly as critical as clinical judgment, and for good reason. Poor prioritization creates a domino effect: safety protocols get rushed, clinical judgment suffers under cognitive overload, documentation falls behind, and patient interactions become transactional.
Here's the brutal reality: new nurses are being asked to master time management in conditions that would challenge even veterans. Chronic understaffing means the nurse-to-patient ratios that should allow for learning are rare. The challenge isn't working faster, it's developing the instinct to know which patient needs attention first when three call lights go off simultaneously, what can safely wait versus what cannot, and when to ask for help before you're overwhelmed.
This isn't about personal failing. It's about being thrown into triage-level decision-making on day one without the experience to back it up.
3. Teamwork and Collaboration
Nurses don't work in isolation; they coordinate with physicians, pharmacists, respiratory therapists, social workers, and more. With 60% of hiring leaders citing this as essential, teamwork has become a cornerstone of practice readiness.
It's also where new nurses struggle most. Nearly half (47%) cite limited interdisciplinary experience as the top onboarding headache—the single most commonly reported gap.
The problem is having the confidence to speak up when a physician's order doesn't match the bedside reality, or knowing how to escalate when a consult is delayed and the patient is declining. New graduates understand SBAR in theory but haven't practiced navigating the power dynamics and rapid-fire handoffs of real interdisciplinary care.
When collaboration breaks down, patients fall through the cracks. Labs get missed. Pain goes unmanaged. Medication errors slip through.
4. Safe Performance of Core Bedside Procedures
Hand hygiene before and after every patient contact, sterile technique during line changes, and two-person verification before blood transfusions are baseline protocols that prevent infections, medication errors, and patient deaths. Nearly 60% of hiring leaders want nurses who perform these protocols flawlessly, even when everything else feels like it’s on fire.
Here's where new graduates falter: maintaining those standards while juggling five patients, three of whom are unstable. It's easy to skip the second ID check when a new nurse is running behind and the patient is in pain. To contaminate a sterile field when they’re interrupted mid-procedure by a rapid response call down the hall. To forget hand hygiene between rooms when call lights are going off and they’re drowning.
But those "small" lapses aren't small. They're how a medication meant for Room 12 goes to Room 21. How C. diff spreads through a unit. Especially in high-acuity environments where margins are razor-thin, one missed step can spiral into serious harm, or worse.

5. Stress Management and Resilience
Half of all hiring leaders now consider stress management essential and it's clear why. Today's nurses face chronic understaffing, higher patient acuity, and the weight of life-and-death decisions made under relentless time pressure.
But resilience isn't about avoiding burnout. It's about maintaining clinical excellence when they’re on hour twelve of an understaffed shift. It’s keeping their hands steady for an IV start even though they missed lunch and staying sharp enough to catch a dosing error when the EHR screen is blurring.
When resilience breaks, everything else falls apart. Clinical judgment deteriorates. Safety protocols get missed. Communication turns curt. The nurse who walked in ready to provide excellent care leaves feeling like they failed. Stress doesn't just impact every other competency on this list. It determines whether nurses stay at the bedside at all.
Yet there's one competency that's evolved faster than all the others combined, and it's reshaping what 'practice ready' even means.
6. The Rapid Riser: Technology Fluency in an AI-Transformed Landscape
Perhaps no competency has evolved as rapidly as technology fluency. Three years ago, AI-assisted charting was a nice-to-have skill. Today, 69% of hiring leaders consider it essential - a staggering 165% increase in expectations in barely three years.
Hospitals now expect new graduates to handle AI-driven documentation and clinical decision-support tools with minimal training. Magnet-designated hospitals set an even higher bar, with nearly twice as many expecting day-one mastery.
Here's the silver lining: new graduates are often ahead of more experienced colleagues when adopting AI-assisted tools. But there's an important caveat: technology isn't replacing nurses, it's amplifying human expertise. The vast majority of facilities using AI report that it raises the bar for clinical judgment rather than replacing it. Nurses who can't effectively use these tools won't lose their jobs to AI, but they will struggle to keep pace with colleagues who can.
"Patients and families will always want the human touch. Being in hospital is very stressful. AI cannot show empathy and compassion." — Manager, Human Resources at an Integrated Health System Facility
Closing the Gap Together
The divide between classroom preparation and clinical reality is playing out in real time. Fifty-six percent of hospitals have watched at least one bedside position remain unfilled for three months or longer. When new nurses aren't practice-ready, patients wait longer for care, experienced staff burn out faster, and the graduates themselves leave the profession disillusioned.
But change is possible right now.
Nearly every hiring leader surveyed (98%) wants closer partnerships with nursing schools. And they're willing to pay for it - 95% say their facilities would fund tuition support, scholarships, or residency stipends to make it happen. Three-quarters agree that integrating high-fidelity simulation could safely shorten nurse residency programs by roughly a month without sacrificing competence.
The path forward isn't just theoretical. Schools that embed experiential learning—VR scenarios, interdisciplinary labs, AI-enabled charting practice—are already producing graduates who hit the ground running. Hospitals that co-develop curriculum with local programs are finding the confident, practice-ready nurses they desperately need.
The gap is real. But it's closeable.
Programs that weave these six competencies into every clinical scenario will send out graduates who feel at home in modern healthcare. Hospitals that invest in these partnerships will build the agile, technology-fluent care teams that tomorrow's patients demand.
UbiSim's VR simulation platform is already helping nursing programs close this gap, providing the high-fidelity, repeatable practice that builds these six competencies before students ever step on a hospital floor.
Ready to dive deeper? Download the full research report for detailed breakdowns of:
- Regional insights: US vs. Canada competency gap analysis
- Magnet hospital benchmarks: AI fluency standards
- Partnership playbooks: Models already working
- VR scenario library: Time-management accelerators
- Infrastructure ROI: Shared simulation lab calculations
FAQs
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript
The top five competencies are clinical judgment and critical thinking (69%), time management and prioritization (67%), teamwork and collaboration (60%), safe performance of core bedside procedures (59%), and stress management and resilience (50%). Technology fluency has surged 165% in three years, with 69% of hiring leaders now considering it essential.
New graduates excel at textbook knowledge but struggle applying skills under pressure. Sixty-five percent of hospital leaders say finding practice-ready graduates is harder than three years ago. The biggest gap is limited interdisciplinary experience (47%), followed by difficulty recognizing early patient deterioration (64%).
Fifty-six percent of hospitals have had bedside positions remain unfilled for three months or longer. Beyond vacancy costs, hospitals invest in extended orientation programs, manage increased patient safety risks, and lose new graduates to first-year turnover when the training-to-reality gap feels insurmountable.
Yes. Seventy-five percent of hiring leaders agree high-fidelity simulation could safely shorten nurse residency programs by approximately one month without sacrificing competence. VR provides repeatable practice building critical competencies before students reach hospital floors, reducing orientation time.
Yes—98% of hiring leaders want closer partnerships with nursing schools, and 95% would fund tuition support, scholarships, or residency stipends. Schools embedding experiential learning like VR scenarios and interdisciplinary labs already produce graduates who arrive practice-ready, reducing hospital orientation costs.
Explore more

Why Q1 Decisions Determine Your Nursing Workforce Pipeline
Why January–March decisions shape nursing workforce capacity, readiness, and retention, and how early action strengthens the pipeline.
.png)
From 30 Minutes to 3: How AI Enhanced Analytics Transforms Debriefing Preparation
AI Enhanced Analytics: Scenario Performance Data now available in UbiSim's Version 1.19
.jpg)
Behind the Scenes: How We Brought Incisions & Dressings to Life in VR
How the UbiSim team built a VR system displaying 300+ distinct incision states—balancing clinical accuracy, technical constraints, and nursing education needs.


