How UIW Systematically Made VR Simulation Psychologically Safe for Every Student
Table of Contents
Name of the heading 1
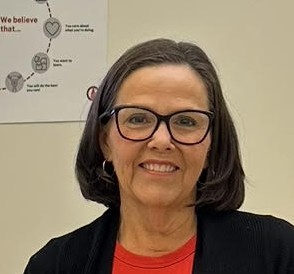
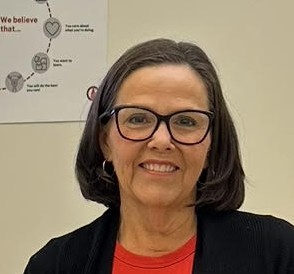
Cynthia Voyce, EdD, MSN, RN, CHSE, Simulation Director at the University of the Incarnate Word, remembers the student who approached her after experiencing VR simulation for the first time. The student struggled with performance anxiety and typically dreaded traditional simulation days. But this time was different.
"She said, 'I have performance anxiety and I don't like simulation because it makes me anxious,'" Dr. Voyce recalls. "And she said, 'But when I'm in VR, I know that I am being watched, but I don't feel like I'm being watched. And that lets me think about what's happening.’"
That moment revealed what UbiSim naturally creates: an immersive environment that can dissolve the performance anxiety that paralyzes students in traditional simulation. But UIW's team also understood something crucial: the psychological safety that VR offers is fully maximized when an institution builds systems around it that make learning in VR accessible to every student.
Since launching UbiSim in Fall 2024, UIW has built a systematic approach to unlocking that psychological safety for hundreds of nursing students, without missing a single one.

“When learners are avatars in UbiSim, they no longer worry about the normal anxieties of simulation. They are in the hospital room. They are nurses.”
1- Start your table with the syntax {start-table}
2 - Add an H3 Heading to create a new column (this will be the column title)
3 - List cells as bullet points in a List element
4 - End your table with the syntax {end-table}
Key Takeaways
- Maximized immersive access: Elite head straps and counterweight batteries enabled every student, even those prone to motion sensitivity, to experience full VR immersion.
- Built feedback loops with clinical faculty for customization: Used clinical instructors to identify what students might encounter in real life and updated scenarios to match current practices.
- Protected safety through standards: Mandatory faculty training and a structured facilitation approach ensured that psychological safety extended throughout pre-brief, sim, and debrief.
Ensuring Every Student Could Experience Full Immersion
While students can participate by watching simulations cast to a screen, UIW wanted every learner to experience direct immersion in the VR environment. Most students adapted easily to it, but some were worried about experiencing motion sensitivity. UIW's response was to invest in hardware that would support every student, regardless of their individual tolerance.
Their solution: Replace standard Meta elastic straps with Elite straps and extended batteries. "The battery sits back on your head, and it counteracts the weight on your face," Dr. Voyce explains. "Being able to secure the goggles so they’re not wobbling around reduces the chance of cybersickness."
The adjustments made a difference for students who initially experienced discomfort. Jill Lear, BSN, RN, Clinical Teaching Assistant, helps faculty support any students who need adjustments, and she shared, "Students who have said, 'Oh, I can't do VR at all. I get cyber sick,' then they get in UbiSim with our setup, and they are okay.”
The result: "We haven’t had any student who could not complete their VR sim," Dr. Voyce says. "They all eventually got in and were successful."
.jpg)
Designing for Universal Engagement
With hardware enabling full immersive access, UIW turned to pedagogy. Traditional simulation structures often left students disengaged or allowed some students to step up and others to step down, determining who practiced and who watched.
"Our clinical groups are eight students, and we bring them all in," Dr. Voyce explains. "With software before UbiSim, we would have two people, maybe three people in the goggles because that's all you could put in the sim. And the other five were watching and they were not engaged."
The breakthrough came from adopting UbiSim and gaining access to peer-facilitated simulation. UIW pairs students: one in the VR headset as the caregiver, one at a laptop as the facilitator. Critically, only one student enters the virtual patient room at a time.
"We don't put two people in the room at one time," Dr. Voyce says. Her experience is, "If you put multiple people in a room in simulation, whether it be a face-to-face or virtual, there's going to be a wallflower somewhere and they're going to be standing back doing nothing."
Dr. Voyce explains, "We no longer have the case where students defer to somebody else. Instead, they have gotten comfortable doing things in UbiSim VR, and they're able to make more decisions and think through the scenario on their own."
Gracie Baylor, MSN, RN, Clinical Teaching Assistant, observes this confidence-building in real time. "Students are engaged, and they don't seem to feel that pressure while they're in there with all eyes on them. They're in VR independently taking care of the patient.”
Dr. Voyce connects the pedagogy back to the psychological safety that the first student described. "Students get anxious in front of a camera in the sim lab; Is their hair right? Is their shirt wrinkled? All those worries… When learners are avatars in UbiSim, they’re no longer worried about those normal anxieties of simulation. They are in the hospital room. They are nurses.”
Protecting Psychological Safety Throughout the Experience
VR's immersive environment offers psychological safety during the simulation itself. But the full learning experience includes pre-briefing and debriefing, and without consistent, trained facilitation, that safety can be more challenging.
Dr. Voyce understood that hardware and pedagogy needed a foundation of quality standards to protect psychological safety at every stage. The non-negotiables were clear: "If you're going to facilitate VR, you must do the training. You must be evaluated, and you must adhere to a structured pre-brief and debrief."
The investment paid off. UIW secured grant funding for training and systematically prepared its faculty. "We currently have trained 28 faculty and staff trained to facilitate virtual sim," Dr. Voyce reports.
Gracie plays a central role in that training, covering both the technology and the pedagogical approach. "I help train the faculty on VR using the headsets and getting into the simulation piece. We go through the UbiSim scenario from start to finish to help the faculty become familiar with what the students can see.”
The curriculum integration was equally strategic. "We adopted VR simulation as part of our curriculum," Dr. Voyce explains.
This institutional structure created real flexibility for students who needed accommodations. "Last year, we had a student on maternity leave. We sent a VR headset home with her. While her baby was sleeping, she did her clinical simulation from home with her instructor facilitating from school."
The Results: Rapid Scale with Universal Success
When asked what she'd tell another school considering VR, Dr. Voyce didn’t hesitate: "I would say definitely do it. The flexibility is there. There’s going to be an initial investment, like with anything. And you have to have the plan to implement it. But it’s worth it."
VR simulation offers inherent psychological safety: the immersion, the avatar, the opportunity to make mistakes without harming a real patient. But UIW's experience shows that it is optimized when a nursing program systematically builds the infrastructure, pedagogy, and standards that enable every student to access it.
The anxious student who could finally think clearly in the headset? That was UbiSim - but it was also thoughtful hardware choices, intentional pedagogical design, and unwavering commitment to training faculty and students all working together.
The result? Students who practice independently, make clinical decisions confidently, and enter clinical rotations better prepared. UIW's systematic approach transformed VR's promise of psychological safety into a consistent reality across hundreds of nursing students.
"Last year, we had a student on maternity leave. We sent VR goggles home with her. While her baby was sleeping, she did her clinical simulation from home with her instructor facilitating from campus."
Explore more

How SELU Uses VR to Prepare Learners for Abnormalities They Can't Practice on Peers
SELU uses UbiSim VR to expose nursing students to abnormalities impossible to practice on peers—resulting in measurably better clinical performance.

How UFV Scaled a VR Simulation Program Across Six Years—and Counting
Discover how UFV scaled UbiSim VR in its BSN program over 6 years to fill clinical gaps, build student confidence, and support long-term skill growth.
.jpg)
Mastering Protocols and Communication in VR Before Becoming a Real Nurse: Michael’s Story
Mastering protocols and communication in VR gave Michael the confidence to become a nurse and pursue a future in functional medicine.



